On a Monday evening in July, armed fighters came to Fondioaga village in eastern Burkina Faso and killed a man. The next morning, they returned, and murdered a second man before continuing their killing spree in a neighboring village. “That was when we realized that if we stayed, they would kill everyone. So we fled with our wives, our children, and our parents,” says 45-year-old O.K.* He escaped with his family to the town of Matiaocoli, 15 miles away. “We left our belongings and animals behind. We don´t know if they will still be there when we return home. Here, we have nothing at all. It is tiring. We are tired with worries.”
The world´s fastest-growing humanitarian crisis is unfolding in Burkina Faso. Over the past two years, escalating violence by armed groups in the north and east of the country has forced more than one million people to flee their homes. Almost half of them have been displaced since the start of this year, following a surge in attacks. Most live in constant fear under precarious conditions, with limited access to water, food, proper shelter, and health care. During the current rainy season, displaced people and host communities face additional challenges, including rising rates of malaria and malnutrition.
Another health issue is less visible, but just as devastating.
“People who have witnessed a violent attack are often traumatized,” explains Doctors Without Borders/Médecins Sans Frontières (MSF) psychologist Issaka Dahila. “First they ask themselves, ‘Why is this happening to me?’ Then they often feel guilty because they survived or they were not able to save others. Their suffering is even worse when they are forced to flee their homes.”
Faced with violence and displacement, people react and adapt in different ways. Some cope through family or community support. Others try to repress and contain their emotions.
“We see people who come to us days, weeks, or even months later with persistent complaints such as sadness, fear, denial, or anger,” says Dahila. “We sometimes hear them say, ‘I´m worthless. My life is meaningless.’ Some people have difficulty seeing a future for themselves. Some even want to end their lives. This summer, a young mother of a one-year-old boy committed suicide after men attacked her village and killed her husband.”
A person’s decision to end their life can be the result of significant psychological suffering that they can no longer sustain. From their perspective, suicide might seem like the only way to stop the pain. Although such cases are rare, they illustrate the trauma that survivors of violence experience. The number of patients with mental health concerns tends to increase during conflicts. According to a study by the World Health Organization, on average five percent of people in conflict areas develop severe mental disorders, and 17 percent develop mild and moderate mental disorders.
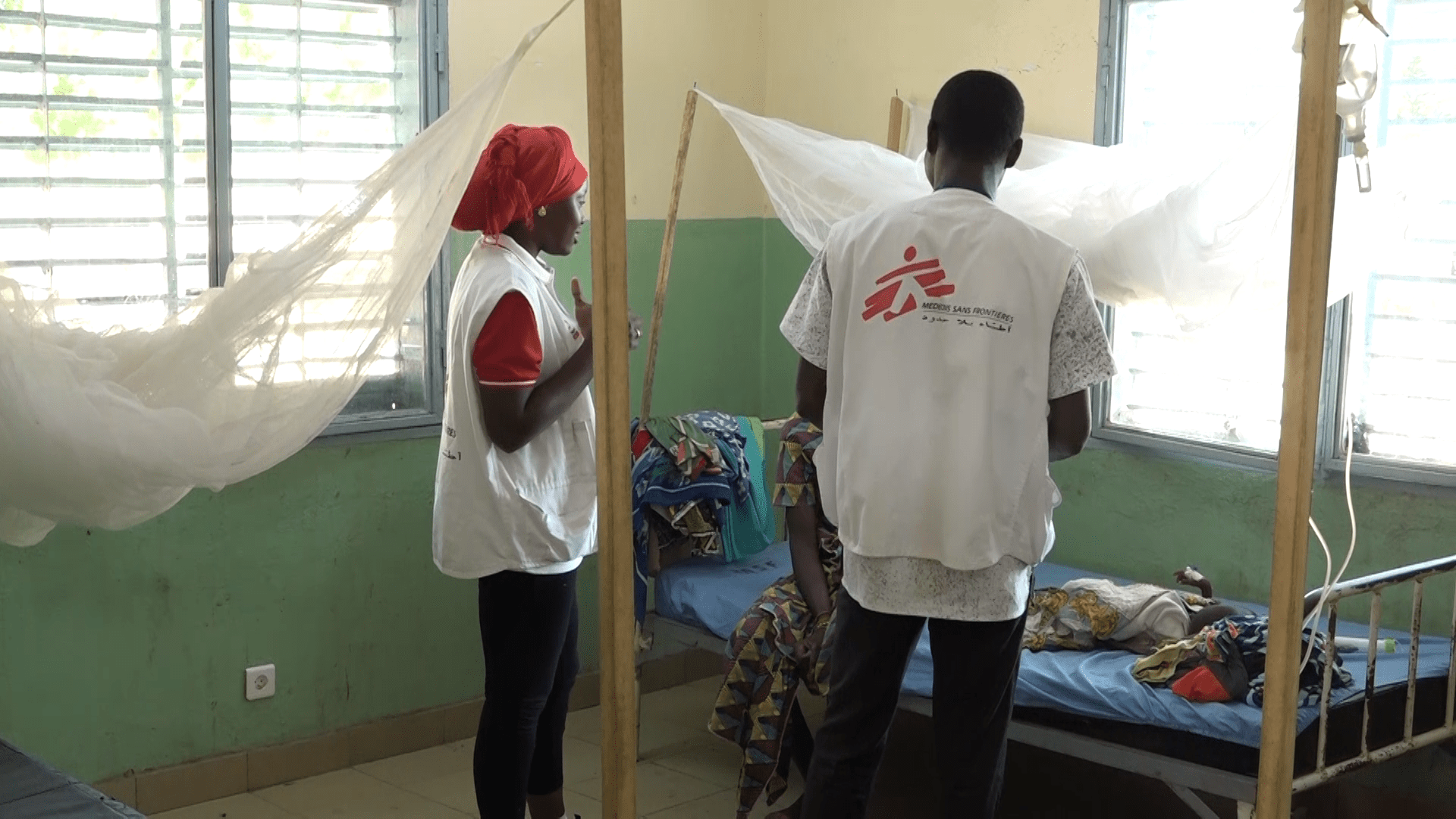
To help ease the suffering of displaced people and host communities, MSF set up mental health services in Burkina Faso’s Eastern region at the end of 2019.
From July to September of this year, 128 people attended individual consultations and 4,391 people participated in group mental health sessions. While some come to our clinics directly to seek help, many get referred from other medical services.
“When we first meet with patients, they describe physical symptoms like sleep problems, headaches, a stronger heartbeat, or feeling startled for no apparent reason. Generally, people are better at identifying physical problems than psychological and emotional ones,” says Dahila. He adds that children have their own way of reacting to the violence and displacement that they have witnessed and experienced. Some show signs of distress with symptoms like bed-wetting and nightmares. They may also use games to reproduce the traumatic event. Others are in denial.
MSF’s mental health team in Burkina Faso offers a number of services to alleviate the psychological suffering of people affected by violence, conflict, or displacement. These include individual, family, and group counseling sessions, where mental health specialists focus on coping mechanisms and building resilience. They also address specific issues and diseases, including sexual violence, HIV/AIDS, and malnutrition. For people who have recently experienced a traumatic event, MSF´s mental health specialists offer “psychological first aid,” a technique designed to reduce the onset of possible psychological trauma.
MSF is holding awareness sessions on the importance of mental health, but not everyone who needs it seeks help. One issue is the difficulty people face accessing mental health services in remote and insecure areas. Another challenge is the stigma that is often associated with mental health issues in Burkina Faso.
MSF began work in Burkina Faso in 1995. Today our teams provide medical and humanitarian assistance to displaced people and host communities in the Sahel, Centre-North, North, and East regions. Services include primary and secondary health care; vaccination campaigns; water, sanitation, and hygiene; and ad hoc distribution of basic relief items. In eastern Burkina Faso, MSF has provided pediatric and maternal health care in two district hospitals and six health posts in Fada and Gayeri since 2019. Our teams also provide mental health services and have set up a network of community health workers trained to treat common illnesses and to refer patients who require urgent medical attention. We have also improved access to water, initially through water trucking and later by drilling and repairing boreholes.
*Name withheld for security reasons