Meanwhile, the suspension of our medical activities ordered by Cameroonian authorities in the Northwest region in December 2020 remains in place, meaning that these two anglophone regions, which have been engulfed in conflict since 2016, have been left without much-needed support.
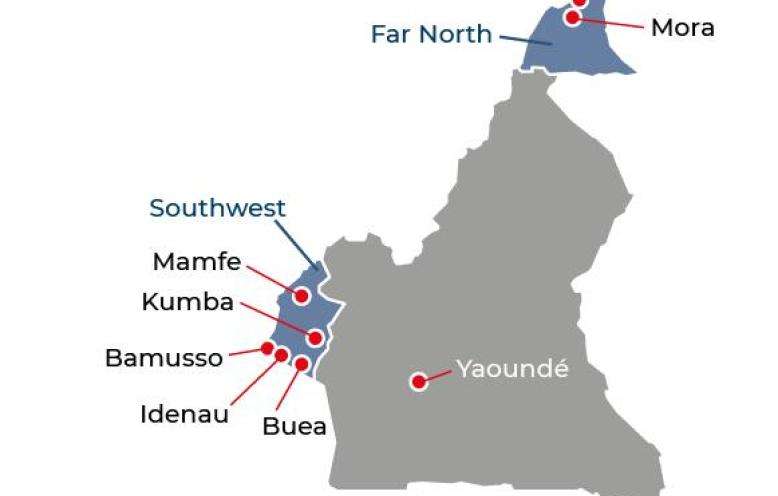
In the Far North region, we responded to the increasing health care needs by treating patients, training medical staff, and reinforcing medical supplies in health centers supported by MSF. We also helped improve access to health care at the community level by working with community health volunteers, whom we have trained to treat simple cases of common diseases.
Heavy rains in Kousseri caused thousands of people to abandon their homes. During the ensuing high peak in malaria, we scaled up treatment in the area. Due to insecurity issues, we made the hard decision to end our activities in Fotokol, where some of our staff were abducted in January 2022.
There was a surge in cholera cases in several regions in 2022. MSF supported the national response in the Centre, Littoral, West and Far North regions, by providing epidemiological surveillance, training community health workers, conducting hygiene activities to curb the spread of the disease, and providing vaccinations. We also supported the national COVID-19 response in the capital, Yaoundé, with testing and vaccinations.