In the first half of 2022, we offered mental health support and training for communities affected by severe floods and landslides in Rio de Janeiro, Bahia, and Pernambuco. With search and rescue activities covered by local authorities, we focused on increasing access to mental health support. Our teams trained health workers, as well as civil servants such as teachers, social workers, and community leaders, so that they could provide psychosocial support to survivors of the disaster, and also create a long-lasting local capacity to enable communities to respond to such events in the future.

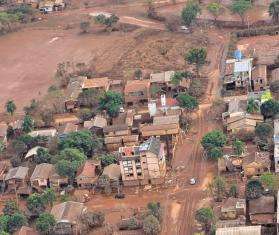
Brazil 2021 © Mariana Abdalla/MSF
Brazil
Improving medical care for Venezuelan migrants, asylum seekers, and the local population.
“We have lost everything. But I am very strong:” Brazilians shelter from flood devastation
June 3, 2024 — A team of doctors, nurses, psychologists, and health promoters with Doctors Without Borders/Médecins Sans Frontières(MSF) is providing medical and mental health assistance to the people from Canoas, which is the state’s third most populous city. “We had no idea of how big this tragedy would be,” said Ana Célia Alves, who now lives in the Canoas’ school-turned-shelter after being rescued by a neighbor with a rowboat. “Suddenly, it was all dark. The lights were out and then we started to realize this flood wasn’t like anything we had seen before. We started receiving messages on the phone, warning us that we had to escape because everything would be flooded.”
Read more
Our work in Brazil
In 2023, Doctors Without Borders/Médecins Sans Frontières (MSF) launched a project in the Marajó Island region to help Amazonian communities overcome obstacles and access health care.

What's happening in Brazil
The end of border closures imposed during the COVID-19 pandemic resulted in a huge increase in new arrivals at the end of 2021. The number of Venezuelans who crossed the border surpassed 160,000 in 2022, more than in the two previous years combined. This placed an additional strain on already overburdened local health care facilities in Brazil.

How we're helping in Brazil
MSF scaled up our response in the northern state of Roraima, assisting with the provision of general health care, health promotion, mental health support, and sexual and reproductive health services, by running mobile clinics in migrant hotspots, shelters and informal settlements in the capital, Boa Vista, and in Pacaraima.
We also provided medical assistance to indigenous communities from Venezuela in rural areas around Pacaraima. These migrants are particularly vulnerable due to the barriers they face in accessing the public health system.

How we're helping
5,520
Outpatient consultations
1,350
Individual mental health consultations
540
Mental health consultations provided in group sessions
*Data from MSF International Activity Report 2022
More news and stories
Learn about MSF’s journalistic roots and our commitment to bear witness and speak out about the plight of the people we treat.

Story Jun 03, 2024
“We have lost everything. But I am very strong:” Brazilians shelter fr...
Read More
Story Mar 18, 2024
Rivers, rainforest, and distance stand in the way of care in the Amazo...
Read MoreLearn about MSF’s journalistic roots and our commitment to bear witness and speak out about the plight of the people we treat.