1: Antimicrobial resistance (AMR) is a major medical problem worldwide—and it’s getting worse.
AMR—when microbes like bacteria, viruses, and parasites evolve and survive despite the antimicrobial medicines, such as antibiotics, used against them—can turn even minor cuts and easily-treatable conditions into life-threating situations.
From war-wounded people in Yemen to newborns in the Democratic Republic of Congo to malnourished children in Niger, teams with the international medical humanitarian organization Doctors Without Borders/Médecins Sans Frontières (MSF) see the impact of AMR every day. In many of the low-resource settings in which MSF operates, resistance is especially common for a variety of reasons, such as limited access to clean water, proper sanitation, and quality health care.
AMR is recognized by the World Health Organization as a major public health threat. It caused 1.27 million deaths in 2019 alone. If nothing is done to curb resistance, it could become the leading cause of mortality with 10 million deaths per year globally by 2050. As the COVID-19 pandemic demonstrated, infectious threats anywhere in the world are a threat to communities everywhere.
While MSF works to prevent and address AMR in the places it works, it is a global challenge that requires cooperation and investments from different countries and sectors. The US has a key role to play in strengthening the global response to increasing rates of resistance.
2. Expanding access to laboratories is key for proper diagnosis.
Diagnostic testing is an essential step in determining which bacteria someone is infected with and which antimicrobial is the right one for their particular condition. Testing is also key for preventing, detecting, and controlling outbreaks and guiding public health decisions. However, in many places where MSF works, there simply aren’t laboratories, testing technology, or qualified specialists like microbiologists.
The US should lend financial and technical support to existing laboratories that can test for resistance and help establish new laboratories and train staff, especially in low-resource communities that may not be able to afford to do so on their own.
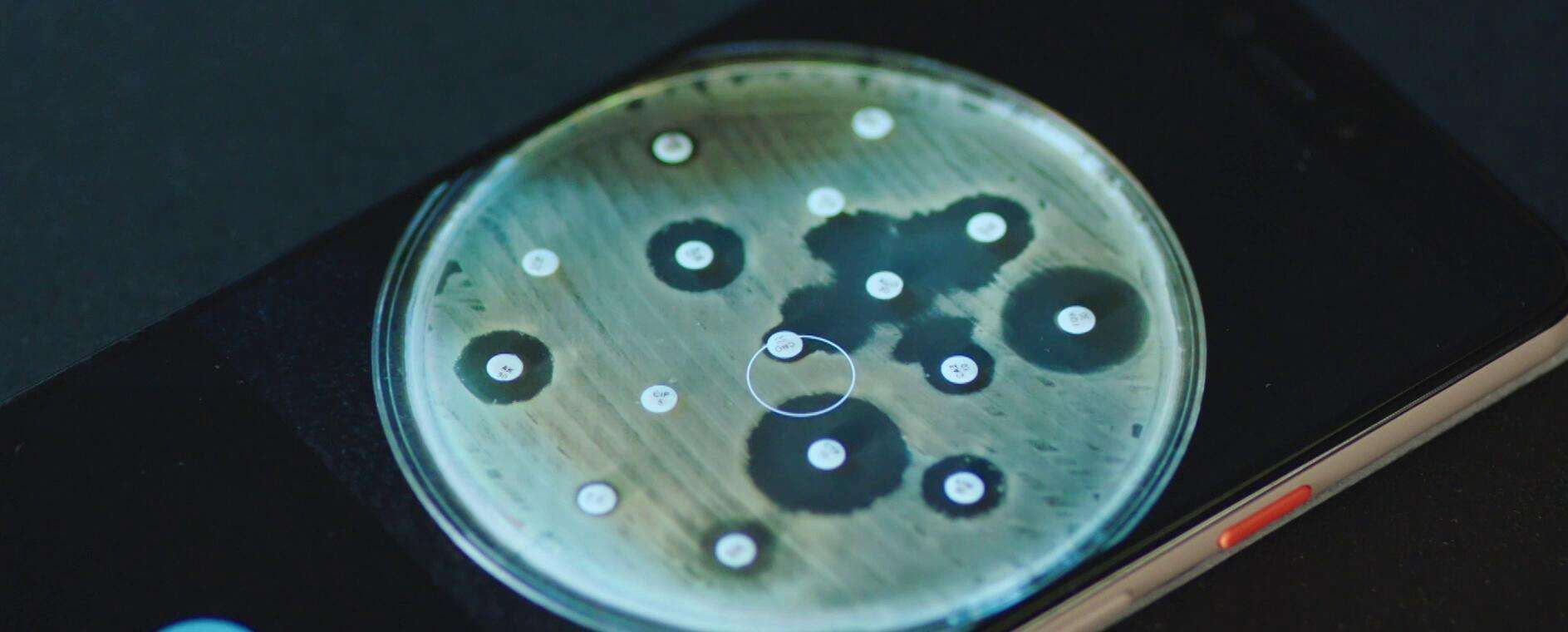
In some settings, innovative approaches are needed to scale up laboratory access. MSF, for example, has developed Antibiogo—a smartphone app that can help laboratory technicians determine if bacteria will respond to particular antibiotics—and the Mini-Lab, which is a simplified, transportable bacteriology laboratory that can be easily assembled where needed and used by non-experts with relatively little training.
3. Infection prevention and control (IPC) and antimicrobial stewardship can help curb the spread of infections and resistance.
Providing access to quality health care is both core to MSF’s mission and essential for combatting AMR.
Infections can spread rapidly without adequate IPC infrastructure, medical tools, and procedures in place in health facilities, such as hospitals built to minimize the potential spread of infections, access to personal protective equipment, and hand-washing facilities and protocols for healthcare workers. IPC is essential for preventing cross-contamination between patients, staff, visitors, and the health care environment; if proper IPC procedures are in place, fewer people will become infected and need antimicrobials.
People with infections should receive the right antimicrobial treatment, like antibiotics, at the right time at the right dose. Not only will this give patients a better chance at recovery, it will reduce the chance of antimicrobial resistance for an individual and in communities. A large proportion of antimicrobials are used inappropriately, however, and rates of antibiotics use are rising most quickly in low- and middle-income countries like those in which MSF operates.
To improve both IPC and antimicrobial stewardship—the appropriate use and administration of antimicrobial treatments—globally, the US should commit resources and technical assistance to help low- and middle-income countries (LMICs) develop infrastructure like health facilities designed to minimize infection risks and train health care workers to prevent infections and only give someone the antibiotics they truly need.
Expanded access to measures that improve communities’ overall health situation and prevent infections more broadly— including access to clean water and sanitation and vaccination—are also key to stemming AMR.
4. Equitable access to existing treatments, diagnostics, and vaccines and ensuring equitable access to future medical tools can help reduce AMR.
People in LMICs experience the highest rates of AMR and infectious diseases globally but are the least likely to have access to medicines, vaccines, and diagnostics. In some cases, this is because the price of medical tools is too high, while in others, tools simply aren’t available locally or haven’t been adapted for use in LMICs (for example, medicines that need to be administered through an IV instead of simply taken by mouth).
As AMR makes existing antimicrobials less effective, there is also a major need for research and development (R&D) for new medicines. Unfortunately, companies aren’t motivated to invest in developing new antimicrobials like antibiotics since they have to be used judiciously and only for short periods of time, making them less lucrative than medicines that large numbers of people might take for the rest of their lives. R&D for diagnostics, especially those that are well-adapted to work in lower-resource settings, is also neglected, despite the key role testing plays in identifying, treating, and containing infections and resistance.
Increasing access to these tools—both existing and yet-to-be-developed—is critical for individual and global health. The US and broader global health community can help LMICs gain sustainable access to existing medical tools by helping countries forecast what they’ll need, making global distribution systems more transparent and responsive, fostering local production, helping countries to band together and procure more affordable medical tools jointly, and providing funding to support this procurement. As the biggest funder of biomedical R&D in the world, the US also can and must take steps to make sure that innovations resulting from that investment are accessible and affordable everywhere they’re needed.

Antimicrobial resistance must be addressed in pandemic preparedness and response
Read the report5. The US must support global action to address AMR.
While the US has a National Action Plan for Combating Antibiotic-Resistant Bacteria (NAP CARB), some countries do not have a plan to tackle AMR and many lack the resources to carry it out. Competing urgent health priorities and a lack of funds in many LMICs have been significant barriers to progress in implementing measures to counter resistant infections. The US should support—through funding, technical assistance, and political support—the development and implementation of national action plans in LMICs.
When countries come together next year at the United Nations High-Level Meeting on AMR, the US should be ready to make strong commitments to address drug resistance at a global level – by coordinating internationally and lending support to countries that face the greatest challenges. Lower income countries, home to many of the communities most directly impacted by AMR, should have leading roles in developing global plans to address resistance.
Higher-income countries like the US must recognize that solidarity on this issue and a collective approach is the only way we prepare for increasing rates of resistance and curb the spread for everyone, everywhere.