In 2003, Guinea was not an obvious choice of location to open an HIV/AIDS project. In contrast to countries at the epicenter of the HIV/AIDS pandemic, like those in southern Africa, where up to one in four adults were living with HIV, just 1.7 percent of Guineans were HIV-positive. But this low prevalence meant that health authorities did not prioritize HIV/AIDS treatment and care among other health needs—and as a result, people had limited access to treatment.
It’s been twenty years since Doctors Without Borders/Médecins Sans Frontières (MSF) opened free HIV testing and treatment centers in Conakry, Guinea’s capital, and began treating HIV patients with antiretroviral drugs. In the two decades since, much progress has been made, but there is still more work to be done in order to reach the “95-95-95" goal set by UNAIDS, which aims to diagnose 95 percent of all HIV-positive individuals, provide ARV treatment for 95 percent of those diagnosed, and achieve viral suppression for 95 percent of those treated by 2030.

“I was sick all the time”
“It was the early 2000s,” recalled Maïmouna Diallo, known as Mouna, who now works with MSF as a community focal point. “I was sick all the time. I saw lots of doctors but no one could tell me what was afflicting me. My older brother, who lived in Europe, helped me financially and took me to England to get tested. [When I tested positive for HIV], although I couldn’t understand what they were saying, I understood it was serious.”
Despite being stigmatized by some relatives, most of Mouna’s family was supportive, especially her brother, who paid for her to get antiretroviral (ARV) medications from abroad. “He said he would help me no matter what, even if he had to sell his house,” she said.
Due to the cost and the difficulty of getting hold of ARVs, some patients went on and off treatment and as a result, developed resistance to first-line medications, making it even more difficult to find an effective treatment regimen.
"At some point, my treatment wasn’t well-tailored anymore,” said Aboubacar Camara, an MSF community educator who is also living with HIV. “I would stop and start. I developed a resistance to the treatment. So, we had to adapt to it."
In 2004, MSF became the first organization to provide ARVs free of charge for HIV patients in Guinea, three years before they were made available for free countrywide.
Over the next decade, the number of HIV patients receiving treatment grew rapidly. Today, MSF cares for 16,425 HIV patients in Guinea, which represents 20 percent of the 86,000 patients on ARV treatment countrywide.

Preventing mother-to-child transmission
From the early days of the program, MSF focused on preventing mother-to-child transmission (PMTCT). “I had two children who were born HIV-negative thanks to the prevention of mother-to-child transmission program,” said Kadiatou Bodié Baldé, president of REGAP+, a community-based organization for people living with HIV. “Today, [my children] are nine and thirteen years old. My daughter knows my status and she is my confidante. I've explained everything to her so that she would not be shocked later. I told her not to touch my blood if I were to cut myself someday. She understands, and she's the one who reminds me to take my medication.”
“MSF’s PMTCT program in Guinea yielded exceptional results,” said Hippolyte Mboma, MSF project coordinator. “As a result of the program, less than 5 percent of children born to HIV-positive mothers have positive status, compared to 20 percent at the national level.”
Innovation in HIV care
A few years into the HIV/AIDS program, MSF realized that, despite providing access to free care and treatment, many people with HIV were still slipping through the cracks. Only one in four Guineans living with HIV were on ARVs in 2012, so mortality linked to HIV remained high.
Advanced care for people who developed AIDS-related complications was available only in a few health facilities, such as the dermatology department at Donka and Ignace-Deen hospitals, both in the capital of Conakry. That’s why MSF opened a specialized care unit inside Donka hospital to help patients with advanced HIV, including people co-infected with tuberculosis (TB) and those in need of palliative care.
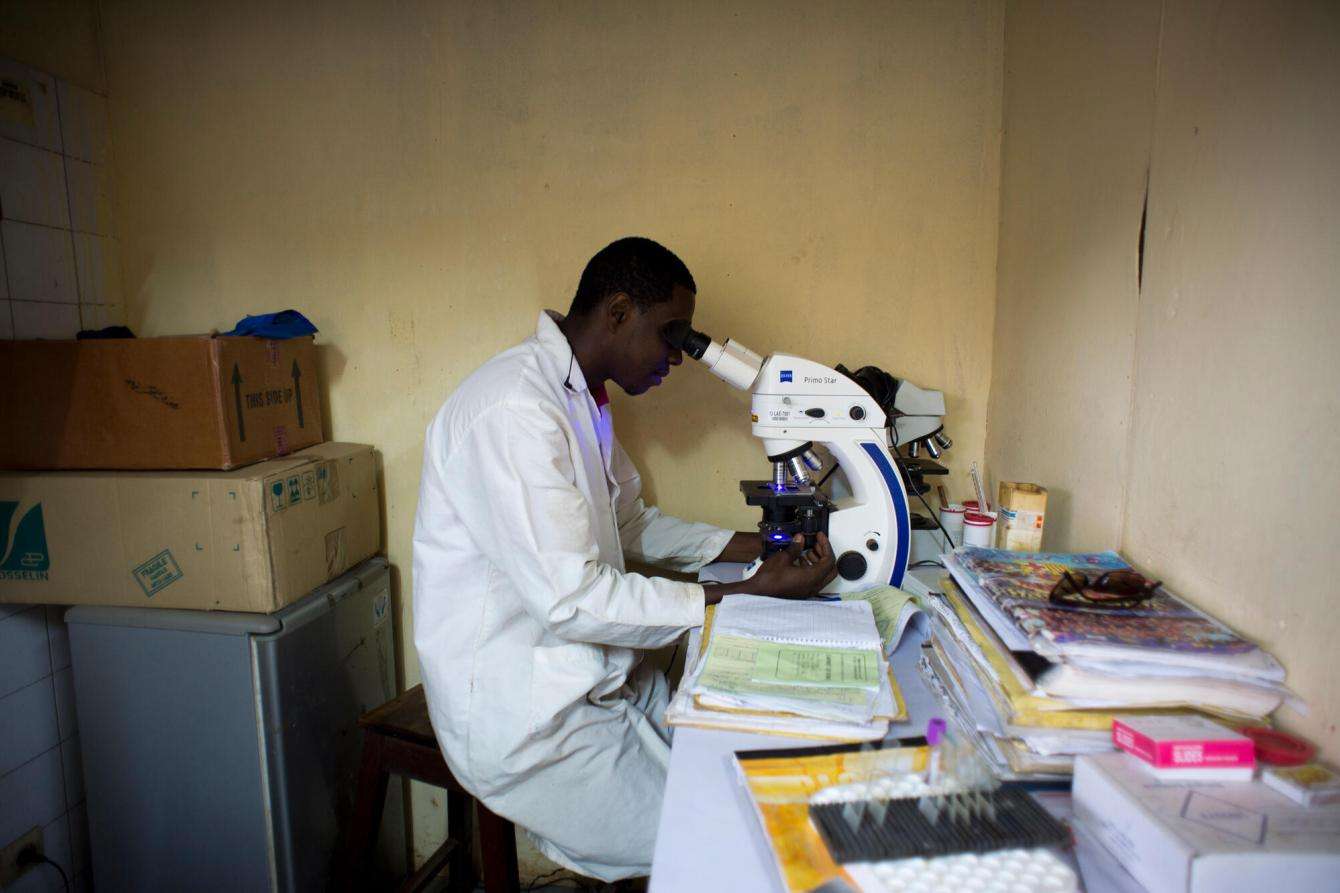
In parallel, MSF piloted the application of the latest HIV treatment guidelines and was one of the first organizations to introduce viral load monitoring in Guinea.
“It isn’t written on our foreheads that we have HIV”
For World AIDS Day, members of MSF’s team in Guinea share insights on living with HIV and fighting stigma in communities.
Making HIV manageable
ARV treatment can make HIV a manageable, chronic condition, allowing HIV-positive people to live long and healthy lives—but only if they adhere to their ARV treatment every day, without fail. This can be more difficult than it sounds, especially if it requires monthly visits to the doctor in a country with few health professionals.
To address the issue, MSF teams in Guinea developed the “six-month appointment program” (known as R6M.3) whereby clinically stable patients receive enough ARV supplies to last for six months, instead of just one month at a time. This cuts the time, costs, and travel needed to access treatment, and allows patients greater autonomy in managing their condition. The R6M.3 initiative proved successful: In 2022, 92 percent of patients enrolled in MSF’s program were still enrolled 12 months later, compared to 61 percent of patients in the regular program.
“When the R6M.3 program worked on our end, the national health program rolled it out nationally,” said MSF’s Dr. Chaloub Souleymane. “The Ministry of Health has become the flag bearer of R6M.3 at the international level.”
In the same spirit, MSF brought into Guinea other successful, simplified models of care developed elsewhere, which decentralized treatment to bring it closer to the community. This included the ARV treatment distribution points first piloted by MSF in Democratic Republic of Congo in 2010 and introduced in Guinea in 2020.
“Simplifying the provision of care for patients while offering specialist medical treatment for advanced HIV were ways to both decrease mortality and improve people’s lives,” said David Therond, MSF head of mission. “But we soon realized that these were not enough, because the level of misinformation, fear, and discrimination were powerful factors preventing people from getting tested and starting treatment. By contrast, seeing HIV-positive people in good health because they have been receiving ARVs is the only truly effective way to change people’s mentalities, decrease stigmatization, and increase demand for treatment.”
MSF worked closely with community-based organizations, community mediators, and patient volunteers who could talk about their condition and, crucially, show that it’s possible to live a long and healthy life with HIV. “It’s not HIV that kills—it’s the stigma and lack of information,” said Mouna.

Peer support: a lifeline for HIV-positive patients
Aboubacar was diagnosed with HIV in 2008. “After I took the test, the doctors stapled a piece of paper to my notes that said: ‘HIV positive.’ They thought I was illiterate. I looked at the paper and fell off my chair. It was beyond me. The doctor prescribed treatment for three months. After three months, I started to get better. Once my prescription ran out, I didn't renew it. I didn't want the entire town to know my diagnosis, but then the disease got worse. I was being stigmatized and discriminated against. I attempted suicide twice. I had no information about the virus. It was the end of my world.”
Peer support was Aboubacar’s lifeline. “One day, I was listening to a show on the radio in which an activist, a peer educator at MSF, was talking about HIV and her diagnosis. She spoke the same language as I did. At the end of the segment, they gave out a phone number. I called it and the next day, I met up with that same activist. She said: ‘If you accept your disease, you will be just like me. I live with HIV, but I’m not going to stop living.’ I found comfort in that group. I even forgot I was sick.”
Since then, Aboubacar has been supporting other patients as a member of a patient-led organization and as an MSF peer educator. He was one of the first people in the country to talk publicly about his status.
“I came up with slogans like, ‘HIV may be in my blood, the struggle against it is in my soul,’” he said. “Today, I'm still helping to demystify HIV in Guinea. My role is to share my experience with other [people living with HIV], to encourage them to accept their illness, and to live positively like me.”
In Guinea, stigma against people with HIV has generally decreased, but it remains a problem in some communities, particularly for sex workers and men who have sex with men. Both groups face difficulties accessing secure testing and care.
Yassine Diallo has worked with MSF since the beginning of the HIV/AIDS project as a maintenance worker and administrative assistant. He is HIV-negative, but talks about HIV prevention to his family, friends, and neighbors without fear. “We can’t choose our diseases, but if I had to choose between HIV and diabetes, I would choose HIV,” he said. “As long as you keep taking your treatment, HIV is no longer a problem. HIV isn’t dangerous with treatment, although it is lifelong.”

The road ahead
Twenty years on, despite the innovations and the progress in HIV care in Guinea, challenges remain in terms of prevention, testing, treatment, and funding.
Today, not all health facilities in Guinea offer free complete care for HIV patients. Due to financial barriers and stigma, many patients still arrive at the MSF-supported HIV unit at Donka hospital in the advanced stages of the disease. There are recurrent stock-outs of ARVs and a sometimes-faulty supply chain. In addition, many health professionals are not sufficiently trained in the management of HIV and comorbidities.
Most of Guinea’s HIV response is covered by the Global Fund to Fight AIDS, Tuberculosis, and Malaria, an international organization that finances the prevention, treatment, and care of these diseases. However, massive gaps remain. Services for preventing mother-to-child transmission are not available everywhere; viral load and early infant diagnosis are not available to all patients; and the screening, prevention, and treatment of opportunistic infections are not available within primary health services.
Children in particular face problems accessing testing and treatment for HIV. Today, 11,000 children under 14 years old are living with HIV in Guinea, and only 3,612 of them are on treatment.
“There are monthly shortages that can occur in pediatric HIV medications, which can lead to backlogs of up to three weeks,” said Dr. Souleymane. “That’s where MSF gets involved: we cover the gaps. Adults and even children can spend weeks without receiving treatment, which can lead to the emergence of [virus] strains that are resistant to ARVs. Some children born to HIV-positive mothers do not have access to pediatric prophylaxis at birth [to prevent transmission], partly because of pediatric ARV shortages, while some other children living with HIV are not on ARV treatment.”
Two decades after MSF launched the HIV/AIDS project in Guinea, we are still one of the key organizations tackling the disease in the country. If the UNAIDS “95-95-95" goals are to be achieved in Guinea, all organizations involved in the testing, treatment, and prevention of HIV/AIDs—including the Ministry of Health, the Global Fund, and other donors—must mobilize and accelerate the current response.




